A new approach to healing headaches: 1 Bioenergetic basis
INTRODUCTION
Why do we experience headache?
Pain as we encounter it in daily life informs us about damage that is happening to the body. Specialized sensory nerves send signals from areas of damage in the skin or inside the body to the brain to inform us that something is going wrong. In other words, pain has a clear life-preserving function, since once we are aware of pain and its cause we can take corrective action to avoid that which is quite literally destroying the body.
But in the case of headaches this life-preserving function of pain seems not to apply, at least with the prevalent types of pain. When headaches appear after a trauma or infection the cause is clear. These so-called secondary headaches generally disappear once the cause has been resolved [1]. However, migraine and tension-type headaches are much more prevalent in the general population. Globally, among adults 11% have current migraine, 42% have tension type headaches and 3% have chronic daily headaches [2]. These types of headache are classified as primary, because common laboratory tests and images cannot identify any pathologic changes in structure or chemistry that are known to induce pain. Primary headaches may occur in what otherwise seems a healthy person.
Migraine very often runs in families and is now generally accepted to be an inherited disease that is genetically transmitted from parent to child [3]. Therefore, it may seem that a person cannot be responsible for her migraine any more than she can be responsible for having a menstrual period.
As a result, primary headaches are generally viewed as an “unfortunate” set of genes or biochemical dysfunction of pain processing system. Naturally, every effort must be made to cancel or suppress the pain. And medication looks, at least initially, like an easy way out. But why then does the pain come back and even get worse with time? A person with headache graduates from generic painkillers to specialised and expensive drugs with a growing list of side-effects that cause major damage to the gastrointestinal tract, the cardiovascular, urinary and nervous systems. Moreover, headache that is caused by medication overuse has become a paradoxical reality for about 1% of the general population worldwide [4]! The behaviour and abnormal brain electrical activity of such frequent users of acute headache medication resembles that of drug addicts (cocaine or amphetamine) [5, 6, 7]. Clearly, the current understanding of headaches and the allopathic methods of treatments have reached a dead-end.
At the same time, from our daily life experience we know that anyone can get a headache after a long day at work or when something really upsets us. We say “Here comes a headache!” when a problem appears with no hope of resolution. How does that tie in with a genetic or mechanistic explanation of headache?
So when I looked at several remarkable healing results of treating headaches with coMra-Therapy, and then researched different insights into the mindset surrounding headaches I started to see the biochemical, psychological and epidemiological evidence of the disease in a very different light. What if headaches are not a meaningless mistake of nature but a biological alarm? Is there a link between mindset, behavioural patterns, neurologic activity, energetic depletion in brain and sensation of pain? And if we can understand what leads to headaches, how can we achieve healing of even the most debilitating headache?
In this article I summarise the evidence of the bioenergetic nature of headaches. I use my own experience of using coMra-Therapy for headache, as well as literature published on the biological processes involved in headaches at a cellular level.
In the following articles I will build on the bioenergetic foundation of headaches and present a holistic view of headaches as a disease that encompass both biology and mindset.
BIOENERGETIC NATURE OF HEADACHES
My own journey that led me to working with headaches started when I used coMra-Therapy to successfully treat a severe headache I had while on a trip in the Andes Mountains in Chile.
“I had about 100 meters left to walk up a steep hill when I started to feel that the lightheadedness I had in the morning was turning into a raging monster. I had to stop every 15-20 steps to gasp for air, but the booming headache was only increasing. By the time I reached the top all I was registering was a blindly sharp headache and my head was ready to explode like a pressure cooker. On a scale of 0 to 10 my headache felt around 9. I did not feel good at all.
It may seem strange why a day of relatively easy hiking in the mountains came to this. But the top of the hill was at 5200 m and it was only my second day since I flew to the Andes from sea level. The headache, fatigue and dizziness I was experiencing were symptoms of high altitude sickness. I did not have enough adaptation and my body was sending me a clear signal what it “thinks” about me, the mountains and the gorgeous view I hoped to be enjoying.
I had high altitude experience and some remaining adaption from a previous short trip to the mountains two months earlier, so I knew what was coming. And yet the headache was still very strong and when I took two tablets of aspirin on the top of the hill they dulled the pain, but it came back in half an hour just as strongly.
In the evening, when I returned to our basecamp at 3700 m, the headache became less sharp (about 7-8) but now I felt even more tired, dizzy and very nauseous. I immediately treated myself with the Delta Laser with an extended Universal 1 Head treatment (16 min) and Universal 3 Blood treatment (10 minutes). In about 5-8 minutes most of the pain was gone! My pain went down from 8 to 1 and I fell into a brief but very refreshing sleep. The fatigue, dizziness and nausea were almost gone, leaving only familiar muscle tiredness. In about two hours I had to repeat the treatment, because I started to feel the headache was about to return, but on the next day I was almost my normal self, without the usual payback for such an experiment on my body.”
This personal experience of the most drastic pain relief got me extremely curious. I had to consider the purely physical/chemical aspect of the pain relief, because in my 19 years of mountain climbing I had never experienced or heard of pain resulting from a serious metabolic disorder, a high-altitude hypoxia, being almost completely removed in a matter of minutes without getting an oxygen mask or strong pain medication. In addition, Oliver Müller published a testimonial of successfully using coMra-Therapy to provide acute pain relief and reduce frequency of attacks in a person with migraine [8]. I saw a strong parallel between these two events and started in-depth research into the bioenergetics of headaches.
HEADACHE AS A SIGNAL OF HYPOXIA AND RESULTING ENERGY DEFICIT IN THE BRAIN Let us use the example of the high altitude headache I presented above.
In cases of too rapid ascent to high altitude, headache is the first sign of a lack of oxygen, a condition known as hypoxia [9]. At 5200 m the atmospheric pressure is only half of that at sea level and every breath taken would have 50% less oxygen. The reason why headache is a hallmark of high altitude is because the brain is extremely sensitive to oxygen supply. Although the brain weighs only 2% of the body weight it consumes 20% of the total energy production [10]. Oxygen is required to maintain stores of the universal cellular fuel (the molecule ATP) that is constantly used to maintain the electrical activity and internal environment in neurons. During rigorous activity such as hiking muscles start to compete for oxygen and reduce even more the oxygen supply to the brain. Hypoxia leads to slowing of ATP production in cells, until a point when all stores of ATP in a cell are exhausted and neurons start to shut down their functionality (from difficulty in thinking to hallucinations) or in extreme cases the cells become permanently damaged (cerebral oedema).
How is the energy deficit in a hypoxic brain expressed as a sensation of pain? Since cellular energy deficit is a common feature of almost all diseases [11, 12], pain could represent an integrated signalling mechanism of the local energetic status of cells. Liedtke presented a conceptual model that explains how energy deficit
in a cell triggers an electrical signal in a nearby sensory nerve that is eventually interpreted as pain [13]. Also, when ATP is released into extracellular spaces it acts as a ubiquitous signalling molecule: practically all cells are sensitive towards ATP and its derivatives [14]. In hypoxic conditions massive amounts of ATP are released into extracellular spaces, where it acts as a pain-relaying messenger [15].
CELLULAR ENERGY DEFICIT IN PRIMARY HEADACHES
We looked at a high altitude headache that was caused by hypoxia and the subsequent energy deficit. But the symptoms I experienced in the high mountains were not too different from classic signs of migraine attack. Is it possible that primary headaches, such as migraine, share the same cellular underpinning of energetic deficit as secondary headaches, such as high-altitude headaches?
First of all, low energy stores in cells can be directly expressed as physical fatigue [16]. Indeed, fatigue is a very common complaint among people with migraine. A study of 63 patients with chronic migraine showed that 84% of them had fatigue and 67% had Chronic Fatigue Syndrome, a very debilitating and persistent fatigue [17]. Prolonged fatigue also often follows a migraine attack in people with episodic migraine.
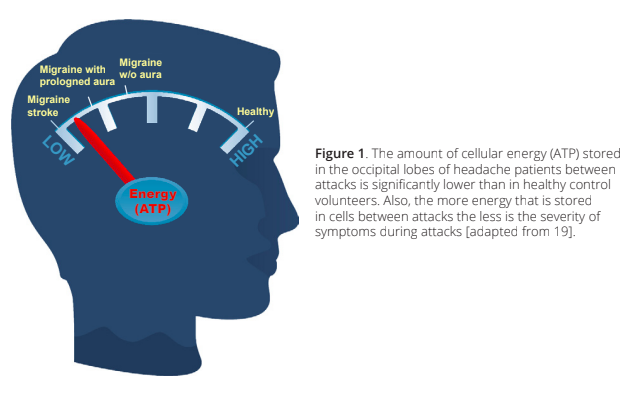
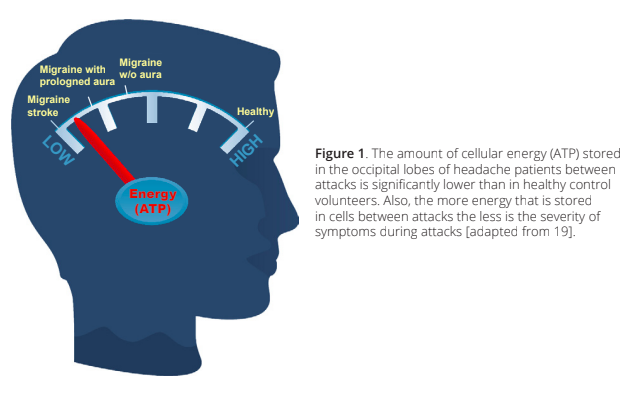
A large body of biochemical evidence collected since 1973 suggested that migraine is associated with impaired energy metabolism [18]. When direct noninvasive measurements, such as magnetic resonance spectroscopy were developed, experiments confirmed that in the brain of people with migraine and cluster headaches the cellular energy stores are significantly lower than in healthy controls [19, 20]. Most notably, the more energy that is stored in cells between attacks the less is the severity of symptoms during attacks (Figure 1).
According to this evidence, an acute migraine attack can be seen as the lowering of energy stores in the brain beyond a critical threshold. Indeed, during a phenomenon known as cortical spreading depression neurons experience a sudden and severe hypoxia, (oxygen drops to 14% of normal levels) and a complete loss of function [21]. Spreading depression is involved in the mechanism of migraine, stroke, subarachnoid haemorrhage and traumatic brain injury [22], and it represents a slowly propagating wave of “silence” of electrical activity and swelling of neurons (Figure 2).
To summarize, the amount of energy stores maintained in cells determines the susceptibility of a person to a migraine attack. A healthy person with significant amounts of energy stores can sustain a great load of energy demand without experiencing pain. In a person with already low energy stores any common disturbance, such as lack of sleep, dehydration, certain foods, smells, sound or menstrual periods can force neurons over a critical energetic threshold, leading to an experience of pain and loss of functionality.
CAUSE OF ENERGETIC DEFICIT IN HEADACHE
Now we come to a key question: what causes energetic deficit in the brain?
Understanding the cause will point out the right corrective action. For example, insufficient oxygen supply to the brain was the cause of my headache in my example above. Therefore, supplementation of oxygen with an oxygen mask, descent to a lower altitude [9] and, as I will explain later, coMra-Therapy will directly contribute

 to the resolution of the cause. It is possible to temporarily suppress the pain by medication, but one must keep in mind that painkillers do not provide additional energy to cells. Medication only interrupts the flow of information about energy deficit by chemically disrupting the pain-relaying chain. If I were to dull my headache completely with gigantic doses of painkillers and then continue climbing higher I risk pushing my body into irreversible damage.
The amount of energy in a cell depends on:
1) Supply of oxygen and glucose to cells;
2) Efficiency of production of the energy-rich ATP molecule;
3) Expenditure of cellular ATP stores for various cellular functions.
Disruption of the supply of materials necessary for energy production was long considered as the main cause of migraine. Constriction of cerebral blood vessels was thought to decrease the amount of oxygen delivered to the brain cells and to cause hypoxia and pain. But now the “Vascular Hypothesis” seems to be largely disproven [24]. However, in the case of tension-type headaches, we cannot exclude the possibility of chronic tension of muscles in the neck and shoulders inhibiting blood flow to the brain.
The second aspect refers to how efficiently the supplied glucose and oxygen are used for the production of ATP inside the mitochondrion, the cellular “power plant”. Electron microscopical studies revealed abnormal structural changes in mitochondria in migraine sufferers [18]. It is well established that such changes reflect
impaired energy metabolism. But no evidence has been found that such changes are associated with genetic mutations in mitochondrial DNA.
Therefore, we need to consider how energy is spent in the brain. Let us go back to the phenomenon of cortical spreading depression that is associated with migraine attacks. The key clue to understanding the cause of energy deficit during an attack was revealed in a detailed study of cortical spreading depression published by Takano et al in Nature Neuroscience [21]:
Our study puts forward a new concept: that a hypoxic state can occur in the absence of reduction in cerebral blood flow under conditions of high energy demand.
Where could such sufficiently “high energy demand” come from to provoke a migraine attack in a person who is just following his or her normal daily routine?
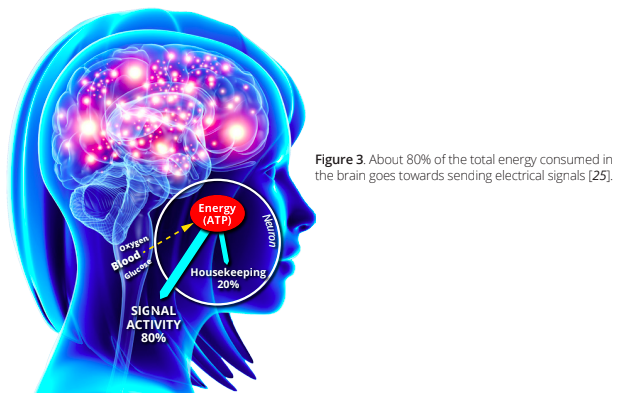
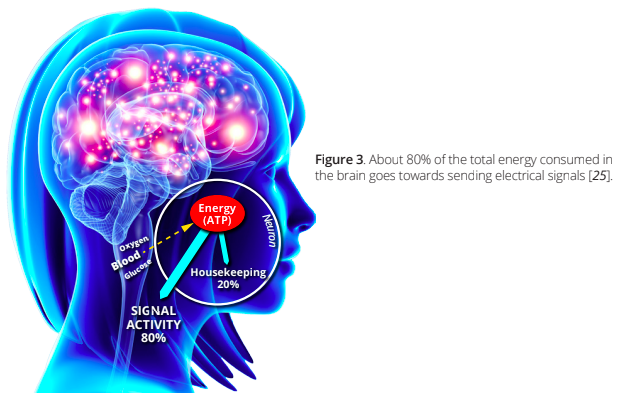
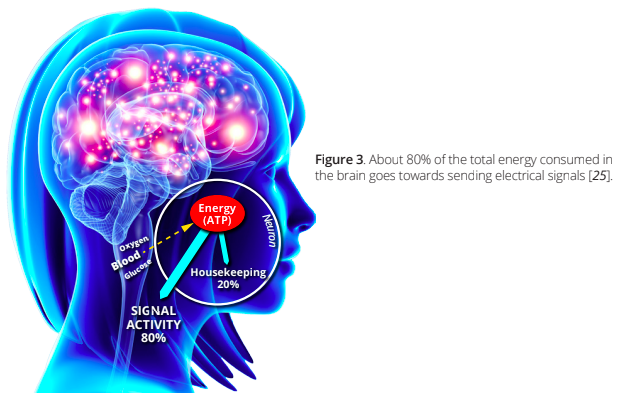
As I described above, neurons consume vast amounts of energy during normal functioning. Of the total amount of energy used by the brain about 80% is used for the generation of electrical signals that travel through the nervous system (Figure 3, [25]). In comparative terms, the energy expenditure of the signal activity in the brain equals the energy usage for a human leg muscle running a marathon [26]! Note that if we are awake and perform no specific tasks, the brain still “runs its marathon” in the background. Only in a deep state of induced anesthesia does brain energy usage drop from the baseline by about 45% [27].
The energy expenditure on signal activity in the brain is not constant, but depends on the level of neuronal activity. Experiments have shown that energy consumption in neurons increases with the frequency of firing of electrical signals [25]. Neurons are activated during sensory activity (vision, smelling, hearing), cognition (thinking, calculating, etc) and motor activity [28].
If we could assume that sensory and motor neural load are more or less the same in the awake state, could it be that in primary headaches the chronic energy deficit is caused by nonstop neuronal activity due to mental and emotional processing in “overdrive”? Just as legs can experience very painful cramps in exhausted muscles during a marathon, what if the brain can experience an acute headache attack when it does not have a chance to rest and recover from elevated energy demand?
I will expand on this question in the following article.
to the resolution of the cause. It is possible to temporarily suppress the pain by medication, but one must keep in mind that painkillers do not provide additional energy to cells. Medication only interrupts the flow of information about energy deficit by chemically disrupting the pain-relaying chain. If I were to dull my headache completely with gigantic doses of painkillers and then continue climbing higher I risk pushing my body into irreversible damage.
The amount of energy in a cell depends on:
1) Supply of oxygen and glucose to cells;
2) Efficiency of production of the energy-rich ATP molecule;
3) Expenditure of cellular ATP stores for various cellular functions.
Disruption of the supply of materials necessary for energy production was long considered as the main cause of migraine. Constriction of cerebral blood vessels was thought to decrease the amount of oxygen delivered to the brain cells and to cause hypoxia and pain. But now the “Vascular Hypothesis” seems to be largely disproven [24]. However, in the case of tension-type headaches, we cannot exclude the possibility of chronic tension of muscles in the neck and shoulders inhibiting blood flow to the brain.
The second aspect refers to how efficiently the supplied glucose and oxygen are used for the production of ATP inside the mitochondrion, the cellular “power plant”. Electron microscopical studies revealed abnormal structural changes in mitochondria in migraine sufferers [18]. It is well established that such changes reflect
impaired energy metabolism. But no evidence has been found that such changes are associated with genetic mutations in mitochondrial DNA.
Therefore, we need to consider how energy is spent in the brain. Let us go back to the phenomenon of cortical spreading depression that is associated with migraine attacks. The key clue to understanding the cause of energy deficit during an attack was revealed in a detailed study of cortical spreading depression published by Takano et al in Nature Neuroscience [21]:
Our study puts forward a new concept: that a hypoxic state can occur in the absence of reduction in cerebral blood flow under conditions of high energy demand.
Where could such sufficiently “high energy demand” come from to provoke a migraine attack in a person who is just following his or her normal daily routine?
As I described above, neurons consume vast amounts of energy during normal functioning. Of the total amount of energy used by the brain about 80% is used for the generation of electrical signals that travel through the nervous system (Figure 3, [25]). In comparative terms, the energy expenditure of the signal activity in the brain equals the energy usage for a human leg muscle running a marathon [26]! Note that if we are awake and perform no specific tasks, the brain still “runs its marathon” in the background. Only in a deep state of induced anesthesia does brain energy usage drop from the baseline by about 45% [27].
The energy expenditure on signal activity in the brain is not constant, but depends on the level of neuronal activity. Experiments have shown that energy consumption in neurons increases with the frequency of firing of electrical signals [25]. Neurons are activated during sensory activity (vision, smelling, hearing), cognition (thinking, calculating, etc) and motor activity [28].
If we could assume that sensory and motor neural load are more or less the same in the awake state, could it be that in primary headaches the chronic energy deficit is caused by nonstop neuronal activity due to mental and emotional processing in “overdrive”? Just as legs can experience very painful cramps in exhausted muscles during a marathon, what if the brain can experience an acute headache attack when it does not have a chance to rest and recover from elevated energy demand?
I will expand on this question in the following article.
 ACKNOWLEDGEMENTS
This article has been inspired by ideas shared with me by Théun Mares. Development of the article has been done with my friends at Radiant Life Technologies.
REFERENCES
ACKNOWLEDGEMENTS
This article has been inspired by ideas shared with me by Théun Mares. Development of the article has been done with my friends at Radiant Life Technologies.
REFERENCES

 to the resolution of the cause. It is possible to temporarily suppress the pain by medication, but one must keep in mind that painkillers do not provide additional energy to cells. Medication only interrupts the flow of information about energy deficit by chemically disrupting the pain-relaying chain. If I were to dull my headache completely with gigantic doses of painkillers and then continue climbing higher I risk pushing my body into irreversible damage.
The amount of energy in a cell depends on:
1) Supply of oxygen and glucose to cells;
2) Efficiency of production of the energy-rich ATP molecule;
3) Expenditure of cellular ATP stores for various cellular functions.
Disruption of the supply of materials necessary for energy production was long considered as the main cause of migraine. Constriction of cerebral blood vessels was thought to decrease the amount of oxygen delivered to the brain cells and to cause hypoxia and pain. But now the “Vascular Hypothesis” seems to be largely disproven [24]. However, in the case of tension-type headaches, we cannot exclude the possibility of chronic tension of muscles in the neck and shoulders inhibiting blood flow to the brain.
The second aspect refers to how efficiently the supplied glucose and oxygen are used for the production of ATP inside the mitochondrion, the cellular “power plant”. Electron microscopical studies revealed abnormal structural changes in mitochondria in migraine sufferers [18]. It is well established that such changes reflect
impaired energy metabolism. But no evidence has been found that such changes are associated with genetic mutations in mitochondrial DNA.
Therefore, we need to consider how energy is spent in the brain. Let us go back to the phenomenon of cortical spreading depression that is associated with migraine attacks. The key clue to understanding the cause of energy deficit during an attack was revealed in a detailed study of cortical spreading depression published by Takano et al in Nature Neuroscience [21]:
Our study puts forward a new concept: that a hypoxic state can occur in the absence of reduction in cerebral blood flow under conditions of high energy demand.
Where could such sufficiently “high energy demand” come from to provoke a migraine attack in a person who is just following his or her normal daily routine?
As I described above, neurons consume vast amounts of energy during normal functioning. Of the total amount of energy used by the brain about 80% is used for the generation of electrical signals that travel through the nervous system (Figure 3, [25]). In comparative terms, the energy expenditure of the signal activity in the brain equals the energy usage for a human leg muscle running a marathon [26]! Note that if we are awake and perform no specific tasks, the brain still “runs its marathon” in the background. Only in a deep state of induced anesthesia does brain energy usage drop from the baseline by about 45% [27].
The energy expenditure on signal activity in the brain is not constant, but depends on the level of neuronal activity. Experiments have shown that energy consumption in neurons increases with the frequency of firing of electrical signals [25]. Neurons are activated during sensory activity (vision, smelling, hearing), cognition (thinking, calculating, etc) and motor activity [28].
If we could assume that sensory and motor neural load are more or less the same in the awake state, could it be that in primary headaches the chronic energy deficit is caused by nonstop neuronal activity due to mental and emotional processing in “overdrive”? Just as legs can experience very painful cramps in exhausted muscles during a marathon, what if the brain can experience an acute headache attack when it does not have a chance to rest and recover from elevated energy demand?
I will expand on this question in the following article.
to the resolution of the cause. It is possible to temporarily suppress the pain by medication, but one must keep in mind that painkillers do not provide additional energy to cells. Medication only interrupts the flow of information about energy deficit by chemically disrupting the pain-relaying chain. If I were to dull my headache completely with gigantic doses of painkillers and then continue climbing higher I risk pushing my body into irreversible damage.
The amount of energy in a cell depends on:
1) Supply of oxygen and glucose to cells;
2) Efficiency of production of the energy-rich ATP molecule;
3) Expenditure of cellular ATP stores for various cellular functions.
Disruption of the supply of materials necessary for energy production was long considered as the main cause of migraine. Constriction of cerebral blood vessels was thought to decrease the amount of oxygen delivered to the brain cells and to cause hypoxia and pain. But now the “Vascular Hypothesis” seems to be largely disproven [24]. However, in the case of tension-type headaches, we cannot exclude the possibility of chronic tension of muscles in the neck and shoulders inhibiting blood flow to the brain.
The second aspect refers to how efficiently the supplied glucose and oxygen are used for the production of ATP inside the mitochondrion, the cellular “power plant”. Electron microscopical studies revealed abnormal structural changes in mitochondria in migraine sufferers [18]. It is well established that such changes reflect
impaired energy metabolism. But no evidence has been found that such changes are associated with genetic mutations in mitochondrial DNA.
Therefore, we need to consider how energy is spent in the brain. Let us go back to the phenomenon of cortical spreading depression that is associated with migraine attacks. The key clue to understanding the cause of energy deficit during an attack was revealed in a detailed study of cortical spreading depression published by Takano et al in Nature Neuroscience [21]:
Our study puts forward a new concept: that a hypoxic state can occur in the absence of reduction in cerebral blood flow under conditions of high energy demand.
Where could such sufficiently “high energy demand” come from to provoke a migraine attack in a person who is just following his or her normal daily routine?
As I described above, neurons consume vast amounts of energy during normal functioning. Of the total amount of energy used by the brain about 80% is used for the generation of electrical signals that travel through the nervous system (Figure 3, [25]). In comparative terms, the energy expenditure of the signal activity in the brain equals the energy usage for a human leg muscle running a marathon [26]! Note that if we are awake and perform no specific tasks, the brain still “runs its marathon” in the background. Only in a deep state of induced anesthesia does brain energy usage drop from the baseline by about 45% [27].
The energy expenditure on signal activity in the brain is not constant, but depends on the level of neuronal activity. Experiments have shown that energy consumption in neurons increases with the frequency of firing of electrical signals [25]. Neurons are activated during sensory activity (vision, smelling, hearing), cognition (thinking, calculating, etc) and motor activity [28].
If we could assume that sensory and motor neural load are more or less the same in the awake state, could it be that in primary headaches the chronic energy deficit is caused by nonstop neuronal activity due to mental and emotional processing in “overdrive”? Just as legs can experience very painful cramps in exhausted muscles during a marathon, what if the brain can experience an acute headache attack when it does not have a chance to rest and recover from elevated energy demand?
I will expand on this question in the following article.
 ACKNOWLEDGEMENTS
This article has been inspired by ideas shared with me by Théun Mares. Development of the article has been done with my friends at Radiant Life Technologies.
REFERENCES
ACKNOWLEDGEMENTS
This article has been inspired by ideas shared with me by Théun Mares. Development of the article has been done with my friends at Radiant Life Technologies.
REFERENCES
- Headache Classification Committee of the International Headache Society. 2004. The International Classification of Headache Disorders. 2nd edn. Cephalalgia no. 24:1-150.
- Stovner, L.J., et al. 2007. The global burden of headache: a documentation of headache prevalence and disability worldwide. Cephalalgia no. 27 (3):193-210. doi: 10.1111/j.1468-2982.2007.01288.x.
- Russell, M.B. 1997. Genetic epidemiology of migraine and cluster headache. Cephalalgia no. 17 (6):683-701. doi: 10.1046/j.1468-2982.1997.1706683.x.
- Diener, H.-C., et al. 2004. Medication-overuse headache: a worldwide problem. The Lancet Neurology no. 3 (8):475-483. doi: 10.1016/S1474-4422(04)00824-5.
- Calabresi, P., et al. 2005. Medication-overuse headache: similarities with drug addiction. Trends in Pharmacological Sciences no. 26 (2):62-8. doi: 10.1016/j.tips.2004.12.008.
- Radat, F., et al. 2008. Behavioral dependence in patients with medication overuse headache: a cross sectional study in consulting patients using the DSM-IV criteria. Headache no. 48 (7):1026-36. doi: 10.1111/j.1526-4610.2007.00999.x.
- Coppola, G., et al. 2010. Abnormal cortical responses to somatosensory stimulation in medication overuse headache. BMC Neurology no. 10 (1):126. doi: 10.1186/1471-2377-10-126.
- Müller, O. 2013. coMra-Therapy suspends life-long migraine for 57-year old female patient. Available from http://www.radiant-life-technologies.com/index.php/en/blog/item/255-comra-therapy-suspends-life long-migraine-for-57-year-old-female-patient.
- Hackett, P.H., et al. 2012. “High-altitude medicine and physiology.” In Wilderness medicine, edited by P.S. Auerbach. Philadelphia: Elsevier/Mosby.
- Rolfe, D.F., et al. 1997. Cellular energy utilization and molecular origin of standard metabolic rate in mammals. Physiological Reviews no. 77 (3):731-58.
- Seppet, E., et al. 2009. Mitochondria and energetic depression in cell pathophysiology. International Journal of Molecular Sciences no. 10 (5):2252-303. doi: 10.3390/ijms10052252.
- Straub, R.H., et al. 2010. Energy regulation and neuroendocrine–immune control in chronic inflammatory diseases. Journal of Internal Medicine no. 267 (6):543-560. doi: 10.1111/j.1365-2796.2010.02218.x.
- Liedtke, R.K. 2009. A general theory on pain as an integrated thermodynamic mechanism. Medical Hypotheses no. 73 (1):86-9. doi: 10.1016/j.mehy.2009.01.026.
- Burnstock, G., et al. 2012. Purinergic signalling and the nervous system. Berlin: Springer.
- Burnstock, G., et al. 2012. Purinergic signalling in the central nervous system. In Purinergic Signalling and the Nervous System, 433-581. Heidelberg: Springer.
- Myhill, S., et al. 2009. Chronic fatigue syndrome and mitochondrial dysfunction. International Journal of Clinical and Experimental Medicine no. 2 (1):1-16.
- Peres, M.F.P., et al. 2002. Fatigue in chronic migraine patients. Cephalalgia no. 22 (9):720-724. doi: 10.1046/j.1468-2982.2002.00426.x.
- Sparaco, M., et al. 2006. Mitochondrial dysfunction and migraine: evidence and hypotheses. Cephalalgia no. 26 (4):361-372. doi: 10.1111/j.1468-2982.2005.01059.x.
- Lodi, R., et al. 2001. Deficient energy metabolism is associated with low free magnesium in the brains of patients with migraine and cluster headache. Brain Research Bulletin no. 54 (4):437-441. doi: 10.1016/S0361-9230(01)00440-3.
- Lodi, R., et al. 2006. Energy metabolism in migraine. Neurological Sciences no. 27 (2):s82-s85. doi: 10.1007/s10072-006-0576-0.
- Takano, T., et al. 2007. Cortical spreading depression causes and coincides with tissue hypoxia. Nature Neuroscience no. 10 (6):754-762. doi: 10.1038/nn1902.
- Lauritzen, M., et al. 2011. Clinical relevance of cortical spreading depression in neurological disorders: migraine, malignant stroke, subarachnoid and intracranial hemorrhage, and traumatic brain injury. Journal of Cerebral Blood Flow & Metabolism no. 31 (1):17-35. doi: 10.1038/jcbfm.2010.191.
- Wikipedia. Cortical spreading depression. [cited December 21, 2013].
- Goadsby, P.J. 2012. Pathophysiology of migraine. Annals of Indian Academy of Neurology no. 15 (Suppl 1):S15-22. doi: 10.4103/0972-2327.99993.
- Hyder, F., et al. 2013. Cortical energy demands of signaling and nonsignaling components in brain are conserved across mammalian species and activity levels. Proceedings of the National Academy of Sciences no. 110 (9):3549-3554. doi: 10.1073/pnas.1214912110.
- Attwell, D., et al. 2001. An energy budget for signaling in the grey matter of the brain. Journal of Cerebral Blood Flow & Metabolism no. 21 (10):1133-1145. doi: 10.1097/00004647-200110000-00001.
- Shulman, R.G., et al. 2009. Baseline brain energy supports the state of consciousness. Proceedings of the National Academy of Sciences no. 106 (27):11096-11101. doi: 10.1073/pnas.0903941106.
- Shetty, P.K., et al. 2012. Cellular links between neuronal activity and energy homeostasis. Frontiers in Pharmacology no. 3:43. doi: 10.3389/fphar.2012.00043.